There's an urgent need to digitize pathology services globally – and, in the UK in particular, the introduction of new digital pathology methods is considered a priority.
Funding has been made available by the British Government which can be used to facilitate the migration to digital pathology services within the NHS, but as you'll know if you have already started down this route – it isn’t always straight-forward.
Huge issues need to be addressed in terms of IT performance, system integration, scalability and data storage, before digital pathology solutions can be successfully deployed.
Why the hurry?
Firstly, the move to digital pathology is long overdue.
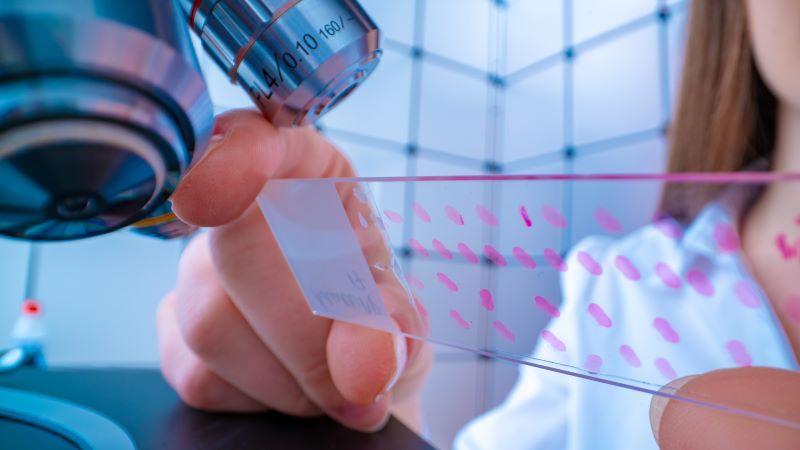
Throughout NHS England, pathology is one of the last remaining analogue processes in the patient care workflow, and traditional methods of analyzing tissues, cells and bodily fluids on a glass slide under a microscope have been unchanged for decades.
Digital pathology solutions allow hospitals to capture high quality images of samples on glass slides – known as whole-slide images (WSI) – which can then be viewed, interpreted, managed and shared digitally.
This digital approach can significantly speed up diagnoses, facilitate faster referrals between hospitals and lead to better health outcomes for patients. There’s no better reason for a speedy change.
At the same time, however, there is enormous pressure on NHS trusts to reform their pathology services as a means of reducing costs and standardizing services across the NHS.
Lord Carter of Coles, in his 2016 report, identified “unwarranted variation” in pathology services within England. He recommended the consolidation of pathology services and the implementation of a more consistent approach to diagnostic services, which can only really be achieved by digitization.
Ultimately, NHS England aims to save around £200 million through this process of reform, so there is understandable impatience for NHS trusts to transform their pathology services.
The key to easy integration and optimum performance
Load balancers are physical appliances or virtual solutions that manage the flow of traffic between applications and servers in a network.
While load balancing capabilities are not generally embedded in most vendors’ digital pathology products, load balancers are nonetheless an essential component of the wider IT environment needed to deliver digital pathology.
Your shortlisted vendors may recommend a load balancer to you, to complement their products, or you may need to source your own solutions.
There are five key ways in which load balancers enable the optimum performance of digital pathology solutions.
They can be used to help you:
1. Keep critical pathology services up and running
Pathology is one of the most critical services provided within the NHS.
Up to 70% of all diagnoses rely on pathology, and over 1 billion pathology tests are carried out each year across 105 hospitals in the UK, according to the Royal College of Pathologists. Given just how important pathology is to patient care, and the sheer number of tests carried out, a top priority for hospital CIOs, CTOs and IT Directors will understandably be reliability. How will you keep this vital service up and running?
Load balancers address this challenge by sharing user traffic across all the available servers and, where appropriate, across all available data centers.
If one server fails, for any reason, the load balancer will automatically direct the traffic to an alternate, functioning server, enabling pathologists to carry on working without interruption.
Equally, load balancers can help provide remote access to digital pathology systems, making it possible for pathologists to work from home or a different hospital and collaborate more easily with colleagues elsewhere in the country to consider complex diagnoses.
2. Facilitate the ‘hub and spoke’ approach
To consolidate pathology services nationally, NHS Improvement has proposed the creation of 29 ‘hub and spoke’ networks, with one primary center supporting pathology services in other nearby hospitals.
This approach is part of the NHS Long Term Plan and aims to make it possible for hospitals to make cost savings by sharing digital pathology systems and other resources, such as skilled pathologists.
Consolidation makes sense, but creates a technical challenge: how can multiple teams, from different organizations securely share the same data and systems?
Load balancers play a key role in multi-site digital pathology deployment models, enabling data to be shared and replicated across several hospitals. They help to preserve the integrity of the data replicated across sites and prevent data loss.
If an outage were to occur in a digital pathology system at one site, it is the load balancer that would step in and redirect user traffic to an alternative location, preventing any interruption in pathology services and delays in diagnoses that could put lives at risk.
3. Alleviate the challenges of system integration
Unchanged for years, pathology departments rely on lots of very old IT systems that are not standardized across the industry and do not integrate well with modern IT. There are even some systems still in use that are written using antiquated programming languages like COBOL.
Consequently, one of the biggest headaches for hospital CTOs, CIOs and IT Directors is integration – how can you make your new digital pathology systems interoperate with the legacy solutions that they will continue to depend on?
This isn’t an insubstantial challenge. IT teams will need to thoroughly investigate all potential integration issues and have a plan for overcoming them, before they start to deploy digital pathology products.
In many cases, load balancers can be used to provide an interface between legacy solutions and state-of-the-art digital pathology solutions.

4. Simplify the management of exceptional data volumes
The digital pathology process generates almost unimaginable volumes of data.
A single 24-bit color WSI has an image size of 15GB, which would typically be compressed to around 300MB. A larger 3D image of a sample, comprising a stack of 10 images, could create a dataset of 3.75TB, which even when compressed would consume 75GB of storage space.
Current guidance stipulates that samples must be saved for at least 12 years, so hospital CTOs, CIOs and IT Directors must think big when calculating the size of their data archives. But it isn’t just the size of the storage that is important – how are you going to handle large image files and ensure that each precious sample is saved?
Hospitals can use load balancers to manage the flow of data into and within data archives to avoid the kinds of failures that can lead to patient data loss.
Load balancers can be used with a hospital’s own vendor-neutral archive (VNA), a data archive supplied by a vendor or a public cloud, such as Azure or Amazon Cloud.
Over time, hospitals are likely to adopt hybrid approaches to image archiving that include on-premise data archives and cloud-based systems, and load balancers can facilitate this model, by directing high volumes of exceptionally large images to the most suitable servers, based on performance and availability.
5. Open the door to artificial intelligence
Artificial intelligence (AI) technology has the potential to accelerate the pathology process dramatically, as it can be used to not only count, but also grade, individual cells in samples, in seconds.
Recognizing this, the British Government has pledged £50 million of further investment for the development of cutting-edge AI solutions to improve diagnosis of disease. This investment should accelerate the availability of proven AI solutions for digital pathology services and make them more viable and available sooner. But, you ask, how easy will it be to actually integrate AI?
In order for AI to work, it needs to receive a lot of data, fast. This means extracting large numbers of image files from archives and feeding them to the AI application in a tiny fraction of a second. Load balancers can perform this data transfer, integrating the two (or more) systems, ensuring that the AI can operate with consistently high performance and high availability.
With the current shortage of trained pathologists (and a large proportion of the workforce approaching retirement), any technology that speeds up the pathology process will be welcome.
Make it easy
According to NHS England and NHS Improvement, “over 97% of all trusts are making progress towards networking their pathology services.” It is probably fair to say, though, that trusts are at very different stages in their journey.
While some NHS trusts have already converged their technology, services and expertise, others are just beginning to have conversations about how to standardize their approach. Deadlines for funding applications in the UK are now looming, so hospital CTOs, CIOs and IT Directors that haven’t yet begun to specify and build their digital pathology systems must soon.
The best advice I can give is: make it easy. You will have the option of purchasing digital pathology solutions as software only, as software and hardware or as a managed service.
If you opt for a managed service, your chosen vendor will be able to advise you on all aspects of your new IT system, including the load balancer, taking away some of the strain of planning your digital pathology deployment yourself – and subsequently managing it.
Digital pathology is such a new field that you are unlikely to have people in your IT team with specialist experience of it. So, lean on IT vendors for guidance and forge ahead with delivering the digital pathology systems your hospital urgently needs.
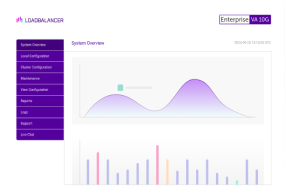
Follow the link to see how to load balance digital pathology applications such as Inspirata Dynamyx.